Background:
Children with sickle cell disease (SCD) are at risk for developing a vaso-occlusive pain crisis (VOC) due to sickled red blood cells causing turbulent blood flow and obstruction within the vasculature, leading to local tissue infarcts and subsequently pain. A VOC can often be managed with analgesics and supportive care either at home or in the emergency room. However, sometimes the pain is not adequately controlled in those settings, so children require hospitalization for further management of their VOC. There exists a high degree of variability in length of hospital stay (LOS) among children who are admitted for VOCs. The purpose of this study is to determine which factors are associated with decreased or increased length of hospital stay (LOS). By identifying these factors, it will allow for a more targeted approach to VOC management with the goal of improving overall pain and reducing LOS.
Methods:
This 3 year (2019 - 2022) retrospective cohort study includes 88 patients (5 years to 27 years of age) with sickle cell disease (HbSS, HbSB0, HbSB+, HbSC) who were hospitalized for VOC management. Several variables were analyzed to determine if they correlated with LOS. These variables included SCD genotype, age, sex, pain scores, average hemoglobin and reticulocyte levels during hospitalization, pain medication dosage and frequency, blood transfusions and complications during hospitalization. The statistical analysis of these variables was conducted across all VOCs of all patients.
Results:
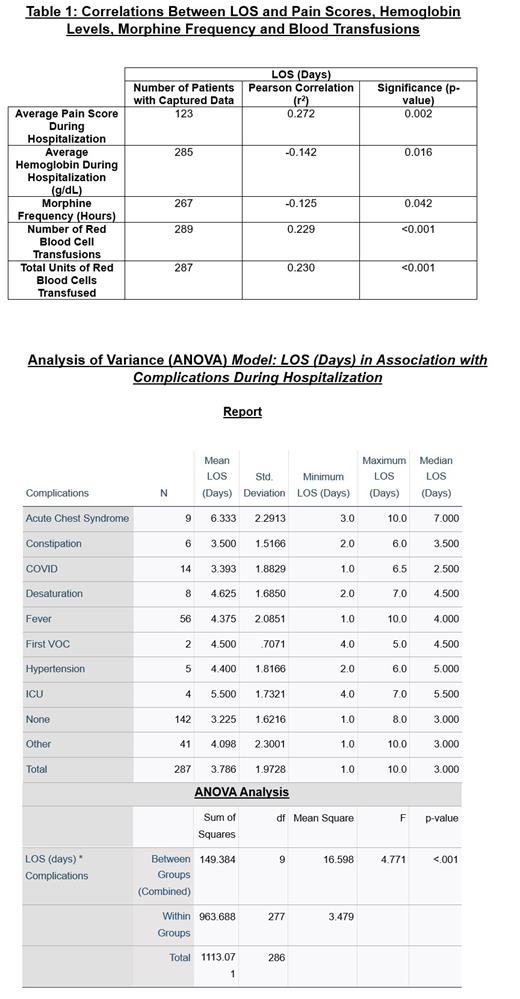
There were 289 hospital admissions for VOCs with a mean of 3.55 hospital admissions per patient among the 88 patients with SCD during study duration. LOS for these VOC hospital admissions ranged from 1 day to 10 days with an overall mean of 3.81 days per hospital admission. LOS was independently highest in females (mean LOS = 4.123 days, F (1, 287) = 6.415, p = .012) and patients who developed acute chest syndrome (mean LOS = 6.333 days, F (9, 277) = 4.771, p < .001). LOS positively correlated with pain scores (r 2 = .272, p = .002), number of blood transfusions (r 2 = .229, p < .001) and total units of blood transfused during admission (r 2 = .230, p < .001) and negatively correlated with morphine frequency (r 2 = -.125, p = .042) and average hemoglobin during admission (r 2 = -.142, p = .016). SCD genotype, age, reticulocyte levels and medication dosage were not found to have a statistically significant association with LOS.
Conclusion:
Our study showed that factors such as higher average pain scores, number of blood transfusions, total units of blood transfused, females and acute chest syndrome were associated with longer LOS. Other factors such as more frequent morphine administration and higher average hemoglobin levels were associated with shorter LOS. While this study provides initial insight into some of the factors that are associated with LOS in children with SCD admitted for a VOC, further studies are warranted to determine if these factors can be used to risk stratify patients in terms of severity of VOC and thereby better optimize and individualize their pain management.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal